Imagine this: You catch a mild bug — something like cowpox — and suddenly, you’re protected against something far more dangerous, like smallpox. Sounds like science fiction, right? Yet that’s exactly how the first vaccine worked. It’s one of the most fascinating quirks of human immunity, and it all comes down to one question:
Can antibodies created for one illness protect you from another?
The surprising answer? Sometimes. But the devil’s in the microscopic details — and not all pathogens play nice.
The antibody puzzle: similar isn’t always the same
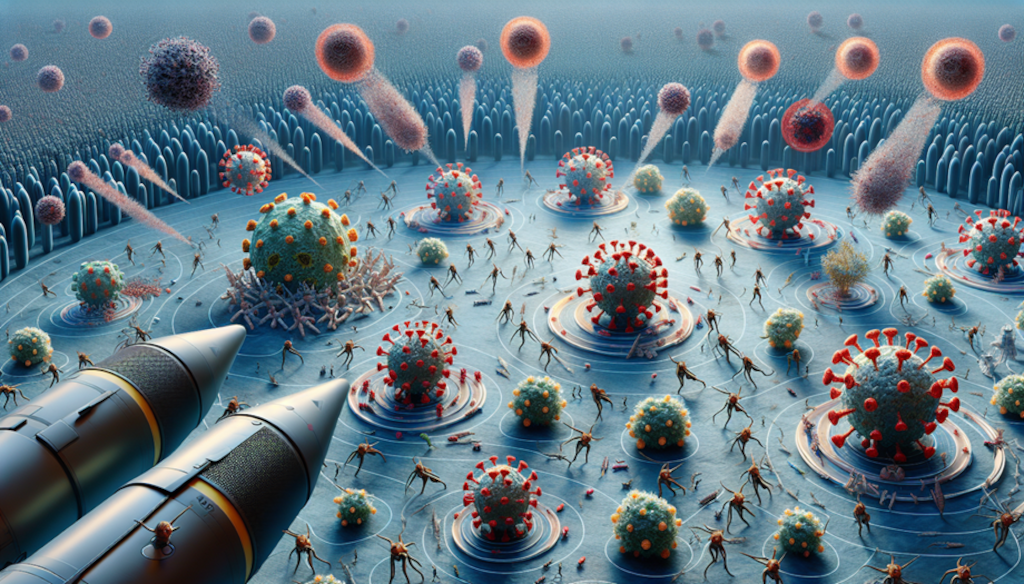
Antibodies are like heat-seeking missiles. Once your body spots an invader — say, the flu — it creates antibodies that are designed to cling to very specific features on that virus’s surface, known as antigens. If two viruses look “similar enough,” some of these antibodies may fit both.
This rare phenomenon is known as cross-reactivity: when antibodies against one pathogen also recognize and attack another.
Sound familiar? Here are some real-world examples:
- Cowpox and smallpox: In the late 1700s, Edward Jenner famously used cowpox to protect people from the deadlier smallpox. Both viruses share similar surface proteins, so antibodies developed against cowpox also fought off smallpox.
- Coronaviruses: Some early studies from the COVID-19 pandemic found that people exposed to common cold coronaviruses had antibodies that partially reacted to SARS-CoV-2. This might help explain why COVID hit some people less severely than others.
- Epstein-Barr virus (EBV): Antibodies made to fight EBV can accidentally target human proteins in a case of mistaken identity, potentially triggering autoimmune diseases like lupus or multiple sclerosis in genetically predisposed individuals.
These cases show that cross-reactivity is real — but they’re the exceptions, not the rule.
Why your body doesn’t “reuse” antibodies more often
Here’s the catch: your immune system is ridiculously specific. Each of us can make up to a quintillion different antibodies. That level of uniqueness means most antibodies are laser-focused on one single enemy.
Think of it like making a key to fit a lock. If the pathogen changes even a tiny bit, your immune system often needs to make a brand-new “key.” Even viruses that are 90% similar may still trick your immune system into starting from scratch.
Interchangeability depends on one thing: antigen similarity
For antibody sharing between illnesses to work, the surface antigens of the pathogens need to be substantially similar. When the epitopes—the small parts of those antigens your antibodies latch onto—are nearly identical, cross-reactivity becomes possible.
But if they’re just a little too different? Your old antibodies just won’t fit the new threat. And worse, in some rare cases, they might even turn against you.
The hidden risk: when cross-reactivity backfires
Cross-reactivity isn’t always helpful. In some cases, it may confuse your immune system into attacking your own cells, leading to autoimmune diseases. For example:
- Some research suggests that antibodies from COVID-19 or EBV may cross-react with certain human proteins, potentially contributing to symptoms like long COVID or autoimmune flares.
In other words, an antibody developed to fight a virus might accidentally declare war on your nervous system. It’s one reason scientists approach antibody therapies with both optimism and caution.
So, can antibodies be shared across illnesses?
In short, only when the threats look alike under a microscope. And even then, it’s risky business.
Here’s what the science says:
- Yes, antibodies can sometimes work on similar illnesses, but only when those pathogens share closely matched structures (antigens).
- Cross-reactivity is rare — it’s the remarkable exception, not the common rule.
- Specificity protects you, but it also means your immune system has to adapt to each new invader — there’s no one-size-fits-all antibody.
- There’s a fine line: some antibodies can accidentally attack your own body, setting the stage for autoimmune disorders.
The bigger takeaway? Your immune system plays a risky balancing act
These tiny defenders — antibodies — walk a razor’s edge between help and harm. Most are incredibly specific. Some are versatile. And a few can backfire. Understanding this helps researchers create better vaccines, safer antibody treatments, and smarter protection strategies for all of us.
So the next time someone asks if your body’s past defenses can protect you from the next big virus, you’ll know what to say:
“Maybe — but it all depends on the shape of the enemy.”



Leave a Comment