You’re sneezing. Your head is pounding. You’re too tired to get off the couch. Sound familiar?
It always seems to start small—just a tickle in your throat. But within days, your entire body feels under attack. Ever wondered how something microscopic can wreak such havoc?
I used to think catching a cold or infection was simple—germs go in, you get sick. But once I started digging into how infections actually spread inside the body, I realized what’s going on beneath the surface is way more complex—and way more interesting.
The surprising point of entry
Here’s the wild part: most infections don’t start with dramatic wounds or gruesome injuries. They usually begin quietly, slipping in through some of your body’s most vulnerable—and most used—gateways.
The top entry points for pathogens (those biological bad guys like viruses, bacteria, fungi, and parasites) include:
- Mucous membranes: Your mouth, nose, eyes, and even genital areas are lined with moisture—perfect spots for microbes to sneak through.
- Respiratory tract: Breathing in airborne particles can invite pathogens straight into your lungs, as we saw with COVID-19.
- Gastrointestinal tract: Ever heard of a stomach bug? Many pathogens get in through contaminated food or water.
- Broken skin: A scrape or bite might seem minor… but to a microorganism, that’s an open door.
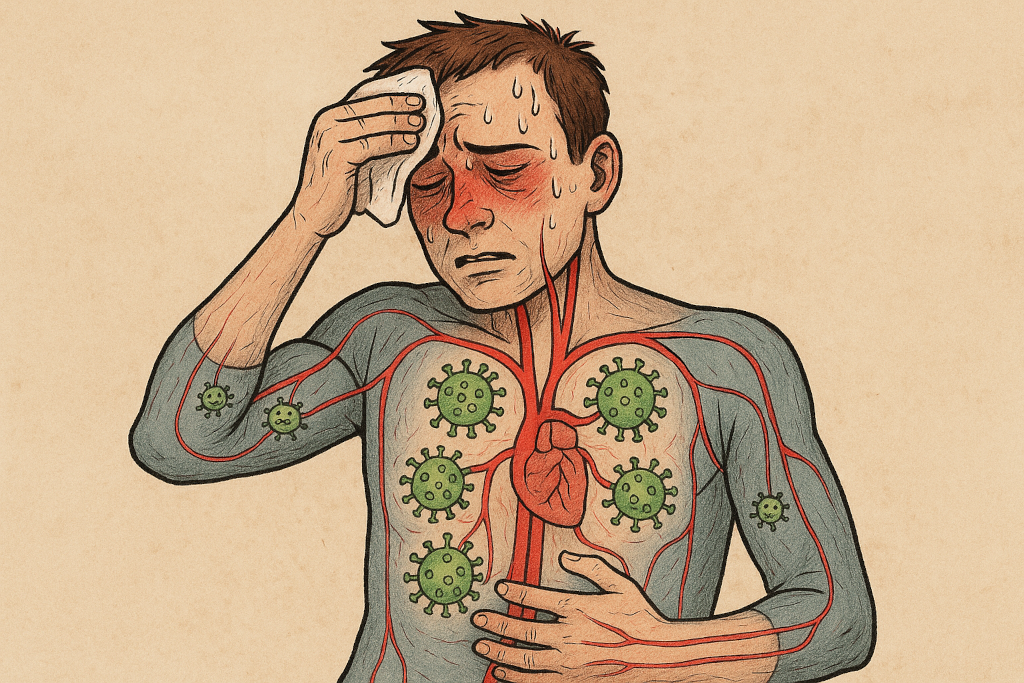
Once inside, the microscopic takeover begins
After entry, the invaders typically start multiplying at the site. Think of it like setting up base camp. Depending on the pathogen, it may stay put—or it may start exploring.
And this is where things get serious. Using your own body’s delivery systems, pathogens can catch a ride and start spreading. How?
- Through the bloodstream: This can lead to conditions like bacteremia (bacteria in the blood) or viremia (viruses in the blood).
- Through the lymphatic system: Like a hidden highway, the lymphatic system can carry pathogens to immunity centers—or around them.
- Along nerves: Some, like herpes and rabies, actually travel via nerve fibers, hiding right under your nose… or skin.
Why don’t we all get equally sick?
One question scientists have long asked: why do some people breeze through an infection, while others land in the hospital?
The answer lies in a tug-of-war between two main players:
- Pathogen traits: How infectious is it (called “infective dose”)? How vicious is it (“virulence”)?
- Your immune system: Are your defenses alert, distracted, or compromised?
During the 2009 H1N1 flu pandemic, it was clear that healthy adults were more likely to recover quickly, while people with weakened immune systems—or with underlying conditions—were more vulnerable to severe symptoms.
Case study: the polio virus’ sneaky journey
Polio, one of the most studied infections in medical history, starts by infecting the digestive tract. But for some, it doesn’t stop there. It travels through the bloodstream and nerve cells, eventually reaching the spinal cord—causing paralysis in its worst cases. Out of thousands infected, a small percentage faced permanent damage. That’s the power (and danger) of systemic infection.
So, what’s the bottom line?
Infections don’t just happen. There’s a biological strategy behind them. From picking the right entry point to hijacking your body’s highways, pathogens are smarter and more dynamic than we often realize.
But here’s the good news: Understanding how infections spread is one of medicine’s greatest tools for preventing them. It’s why we wash our hands. Get vaccines. Avoid touching your face. And why research into viruses, bacteria, and immune responses has exploded in the last few decades.
Think you’re in the clear? Think again.
Here’s the real twist—not all infections make you feel sick right away. Some linger quietly for days, weeks, or even years before causing symptoms. That’s why understanding the infection timeline matters more than ever.
Learning science isn’t just academic. It’s personal. The more you know about how these invisible invaders move, the better you can defend your body from the inside out.
So next time you get that scratchy throat, remember: there’s a war going on inside you. And thanks to science, you’ve got a fighting chance.



Leave a Comment